Non-surgical conservative endodontic treatment of periapical lesions: A prospective study based on intraoral radiographs and clinical findings
By: Dr. Shivangi Singla and Dr. A. K Saigal
 TRUE VALUE DENTAL INSTITUTE
TRUE VALUE DENTAL INSTITUTE
How to cite this article: Singla S, Saigal AK. Non-surgical conservative endodontic treatment of periapical lesions: A prospective study based on intraoral radiographs and clinical findings. IOSR-JDMS. 2021 Aug;20(8):29-38. doi: 10.9790/0853-2008054759
Download Full Pdf
Abstract:
Background: Periapical lesions are the lesions that occur at or around the apex of the tooth as a sequela of chronic pulpal disease. It can be symptomatic or asymptomatic and is generally observed as a radiolucent area which may be well-defined or ill-defined. Management of periapical lesions can be really tough if the etiology and pathogenesis is not known. They can be treated surgically or non-surgically. In this prospective study, treatment of periapical lesions with non-surgical approach is being discussed.
Material and methods:Total 50 cases with periapical radiolucent lesions were treated with the non-surgical conservative endodontic therapy. Clinical observations and radiographs were used to verify lesion size and position, ensuring standard endodontic procedure, and monitoring the progress of bone healing in the lesion area. All cases were selected for statistical assessment on the basis of standard defined parameters after their completion of the follow-up visits over the period of 2 years.Cystic lesions, bony expansion and tumors were excluded.
Results: A success rate of 94% (47 cases) was achieved with nonsurgical management, whereas 6% (3 cases) failed to respond to conservative treatment and had to be subjected to periapical surgery.
Conclusion: Complete healing of the known etiology periapical lesions can be achieved following the nonsurgical conservative endodontic therapy even by using NiTi hand filing approach. in the right sequence and using only normal saline as irrigant and formocresol as antiseptic intracanal medicament.
Keywords: Periapical disease, periapical lesion, radiolucent lesions, periodontal ligament, lamina dura, non-surgical endodontic therapy, periapical healing, prospective study
——————————————————————————————————————-
1. Introduction
Periapical involvement of the bone generally develops as a sequela to pulp disease. It is the chronicity of the carious lesion infecting the pulp that the radiographic changes such as PDL widening and apical periodontitis may occur. Periapical or periradicular lesions are barriers that restrict the microorganisms and prevent their spread into the surrounding tissues; microorganisms induce the periapical lesions, primarily or secondarily.1-2The bone is resorbed, followed by substitution by a granulomatous tissue and a dense wall of polymorphonuclear leukocytes (PMN). Less commonly, there is an epithelial plug at the apical foramen to block the penetration of microorganisms into the extra-radicular tissues.3Larger periapical lesions can also occur without any episode of acute pain and are discovered on routine x-ray examination. Therefore, they may attain a large size before they are diagnosed.
All inflammatory periapical lesions should be initially treated with conservative nonsurgical procedures.4Various non-surgical methods have been used to treat periapical lesions, e.g., orthograde root canal therapy, decompression technique, method using calcium hydroxide, aspiration-irrigation technique, lesion sterilization and repair therapy, active nonsurgical decompression technique and the apexum procedure.5-10 Surgical treatment of these teeth might damage the blood and nerve supply of adjacent teeth, that is why, endodontic treatment of these teeth would be inevitable. According to some reports, surgical retreatments have a higher failure rate11-12 compared to orthograde retreatment. Apical periodontitis lesions, which were treated surgically, healed over 12 months, with healing progress and speed comparable to those treated with non-surgical retreatment modality, plus there was no significant difference in healing rates in the long term. It may imply a higher risk of late failures.13-14 It has its drawbacks; surgery affects the patient’s well-being, with swelling, pain, and discomfort being expected.15 Moreover, many anatomic locations and adjacent structures can affect the feasibility of periapical surgery due to inaccessibility or the risk of damaging adjacent anatomic structures.16 and increased bone loss.5Therefore, to simplify the treatment for such cases, with minimal damage to the adjacent teeth and vital structures, and help conserve the bone, this type of periapical involvement/lesion could be treated non-surgically.It should be considered as an option only in the case of failure of nonsurgical techniques.17
The idea of nonsurgical treatment of periapical lesions is not new. In 1967, Seltzer S et al,18advocated that caries treatment and endodontic therapy should be carried out first to avoid the perpetuation of the interradicular periodontal lesions. In 1972, however, Bhaskar,19described a method of conservative treatment of radicular cysts, which invoked a great deal of controversy, and since then there has been a renewed and sustained interest in this mode of treatment. Similarly, in 2014, Bonaccorso et al,20concluded that sometimes it is difficult to diagnose the disease from pathological alterations. Thus, healing of the endodontic component by effective non-surgical root canal therapy, will allow the exact evaluation of the next treatment procedure, e.g., periodontal therapy or extraction.
So far, many reports of isolated cases being treated successfully by conservative means have appeared in the literature. Results of various retrospective and prospective studies claiming different success rates achieved with nonsurgical management have also appeared.5This approach of conservative treatment of the lesion with judicious planning, is supported by many authors.19, 21-26
However, the present study was planned to determine the success rate achievable with conservative nonsurgical management of periapical lesions through standard endodontic therapy. A thorough clinical examination, radiological investigation, analysis of past and present medical history, pulp vitality tests, and aspiration are essential tools for developing a correct diagnosis of periapical lesions.27-29 Endodontic therapy was undertaken, usingNiTi hand-instrumentation30andonly normal saline for irrigation, to ascertain the success of treatment over the period of 2 years.
Hülsmann (1993) compared the use of hand-instruments and automated device instruments and found that hand instrumentation was superior for the shaping of the root canal. The nearly complete loss of tactile sense during the use of any automated devices was considered and avoidedto prevent possible iatrogenic errors.31In teeth with periradicular lesions, the removal of the irritants (inflamed, infected or necrotic tissue) from the root canal system begins the process of repair and resolution.32 Intraoral periapical radiographs (IOPA) are conventional screening aids, to obtain a view of the entire tooth and its surrounding structures.33The radiographic appearance of the periapical lesions has countless presentations. The clinical challenges in diagnosing and treatment planning, heavily relies on the radiographic changes surrounding the structures of the root.5The film shows the entire crown and root of the teeth and surrounding alveolar bone which provides vital information to aid in the diagnosis of the most common dental diseases; specifically tooth decay, tooth abscesses and periodontal bone loss or gum disease.34 In this study, these radiographic changes along with clinical evaluations, are considered for the healing progress of the periapical lesions.
2. Material and Methods
This prospective comparative study was carried out on patients at True Value Dental Institute, Paschim Vihar, New Delhi, India from March 2018 to March 2021. A total of 50 subjects (both male and female) aged between 15-60 years were included in this study.
Study design: Prospective open label observational study
Study Location: This was a secondary and tertiary care teaching institute-based study done at True Value Dental Institute, Paschim Vihar, New Delhi, India.
Study Duration: March 2018 to March 2021.
Sample Size: 50 patients.
Subjects and selection method: A total of 50 cases, one tooth in each patient, who presented themselves to True Value Dental Institute, with signs and symptoms or radiographic evidence of periapical disease were selected for this study, irrespective of age and sex. All 50 teeth, fulfilled the inclusion criteria. All lesions below 20mm in diameter can be managed with non-surgical treatment as suggested by Natkin et al, 1984.35 Cases were selected in accordance with the normal screening procedures for endodontic case selection between March 2018 to March 2021. Due consideration was given to healthy periodontal support, adequate crown structure for final restoration, and strategic importance of the tooth.
A form was prepared to record each patient’s name, age, sex, address, complete dental history, clinical appearance, and radiographic and vitality test findings at the time of presentation, treatment carried out with number of sittings, date of completion of treatment, and postoperative follow-up recordings after periods of3 months, 6 months, 1 year, and 2 years.
Inclusion criteria:
- Teeth having poor prognosis without endodontic treatment
- Patients aged between 15 to 60 years without any sex discrimination.
- Teeth with nonvital pulps and periapical lesion.
- Lesions below 10mm as seen in the radiograph.
- Cases of periapical abscess or slight bony changes as seen in the radiograph.
- Canals that are completely negotiable for receiving a hermetic seal later.
- The treatment sites were free from any other gross pathology.
- Teeth with completed root formation with mild to moderate root curvatures.
Exclusion criteria:
- Lesions larger than 10mm as seen in the radiograph.
- Patients suffering from debilitating diseases (since their healing potential may have been impaired.)
- Cases of periapical cyst, granuloma, bony expansion and tumors
- Teeth, having malformed or badly curved roots, involved in any gross pathology, non-removable root canal filling or cast post, vertical fracture of the root, root resorption, extra roots, and extremely large or short roots, calcified canals and funnel shaped apices.
- Female pregnant patients.
- Psychological or psychiatric problems.
- Patients on antibiotics or corticosteroids treatment, immunocompromised patients.
- Patients under 15 years and over 60 years of age.

Clinical findings of the involved teeth:
The following clinical findings were examined at every clinical visit.
- All factors of the pain36
- Symptoms and signs of overlying mucosa of the apices (swelling, tenderness to palpation)36
- Reaction to percussion37
- Pus discharge in the canal à It was judged by the color, odor, transparency, and viscosity of the exudate.
- A radiographic examinationà The bisecting-angle technique and SLOB38was employed for all the selected cases.
Protocol:
All the cases were treated by one operator (the chief investigator of the project) so that the factor of personal variation was eliminated. All aspects of endodontic treatment, including irrigating solutions, antiseptic intra-treatment dressings, root canal filling material, and technique, were kept constant to minimize the variables in the present study. All patients were premedicated with antibiotic prophylaxis and NSAID depending on the history of drug allergy, one hour prior to endo-perio therapy.
Non-surgical treatment procedure:
At the first sitting, access to the pulp chamber and deroofing were made by airotor burs for the access opening. The tooth was completely isolated as per the standard endodontic isolation procedure to prevent contamination from saliva and other debris. Next, the root canal was flushed with copious amounts of normal saline39, without any instrumentation, and an antiseptic cotton with Buckley’s formocresol40was used to clean the debris. In the same visit, the root canals were negotiated with sterile #15 and #20 NiTi hand-reamer toextirpate the necrotic pulp tissue and to achieve the glide path with balanced-force technique41-43to promote better irrigation and drainage of pus, if any, from the root canals. Once again, copious irrigation with normal saline was undertaken and an antiseptic dressing of formocresol on cotton was plugged loosely into the pulp chamber, allowing for adequate drainage through the root canal.Above this dressing, a temporary closed restoration with zinc phosphate cement was done to prevent any further contamination of the root canal. The patients were prescribed antibiotics and NSAIDs for 5 days.

After 7 days, in the second sitting, the dressing was checked for any putrid odor, frank discharge and abnormal color change. The root canals were checked for any drainage or debris with a dry paper point. The paper point should be free from any debris or wetting. If symptoms of acute infection had not subsided and the paper point was found to be wet, one more visit was scheduled. In every case, further biomechanical preparation (BMP) was started in the second visit after the determination of the working length. Copious irrigation with normal saline was done again and then #15 and #20 were negotiated again to check the patency of the canals. After this, the root canals were prepared and shaped with NiTi hand-protapers in a balanced-force technique in the proper standard sequence. The protapers ensured the funnel shape of the root canals and better irrigation and filling with an obturating material.
If signs and symptoms of acute infection and abscess were present, apex was prepared till #30 size and the periapical area was punctured with a sharp stroke with #15 or #20 reamer, extending about half the distance in the radiolucent area. Puncturing was done repeatedly two or three times and the area was again flushed well with copious amounts of normal saline. This ensured release of exudative or necrotic material from the periapex through the root canal. after BMP, master cone x-ray with gutta percha was taken.
A maximum of four visits were done. If at the fifth sitting, the infection was still not controlled, as corelated by persistence of discharge or pus, swelling or constant oozing from the canal space, treatment was considered to have failed and the patient was subjected to surgical intervention. If the canal was found fit for obturation at or before the fifth sitting, gutta-percha with zinc oxide as sealer, was placed by the lateral condensation method and a post-treatment radiograph was taken. A permanent restoration was placed at the same time after completing the obturation.
Success criteria: Patients were recalled at 3 months, 6 months, 1 year, and 2 years postoperatively to assess the state of the periapical lesion, both clinically and radiographically. If the tooth was found to be clinically asymptomatic and the radiograph showed disappearance or decrease in size of the periapical radiolucency without any signs for root resorption, treatment was considered to have been successful. If pain or tenderness appeared, if a sinus or swelling developed clinically, if the radiolucency increased in size, or if radiographic evidence of external root resorption was noticed, then treatment was considered to have failed and the lesion was treated surgically.

III. Results
A total of 50 teeth were treated endodontically for periapical disease. There were 15 male and 35 female patients in the age group ranging between 15 and 60 years (Table I).
Mandibular teeth were involved twice as often as maxillary teeth. In this series mandibular anterior teeth were the most commonly affected, followed by maxillary anterior teeth. Mandibular molars were involved more frequently than maxillary molars, and canines were the least affected of all the teeth.
The clinical findings of all the cases at the time of presentation are charted in Table II. Only one patient had intraoral discharging sinus in relation to lower premolar.
There were 4 cases of painless “gumboil,” that is, a small proliferating granulation tissue mass in relation to the apical region of the involved teeth. Ten patients had signs and symptoms of acute apical abscess with severe pain, tenderness, diffuse facial swelling, and mobility of the involved teeth. The remaining 35 cases were diagnosed on routine radiographs taken because of either discolored or fractured teeth or long-standing carious exposures and showed periapical radiolucency of varying sizes.

Of the 50 patients treated, it was possible to follow up 13 (26%) for a period of 2 years,21 (42%) for 1 year, 4 (8%) for 6 months and 5 (10%) for 3 months;4 patients (8%) were lost to follow-up, whereas another 3 patients (6%) were subjected to apical surgery. (Table III)
Critical analysis shows that both failed cases were in premolar teeth. The high failure rate in premolars (all mandibular teeth in this series) could be explained by the fact that maxillary premolars have varied root canal morphology with the presence of apical ramifications and accessory canals that may have remained unfilled and thus caused the failure.
Another observation to be made from the unsuccessful cases is that, even though anterior teeth are easily accessible and single rooted, success is not as easy to achieve as may be assumed. The canals are generally wide, and the apical constriction or the stop is not reliable. Overfilling, underfilling, and incomplete lateral seal are more frequent than in the posterior teeth.

All the unsuccessfully treated patients were subjected to periapical surgery and tissue specimens were sent for histopathologic examination. This revealed that all three, involved chronic inflammatory tissue. According to Prader,44chronic inflammatory tissue in the apical region may sometimes cause resorption of the cementum, and this necrosed cementum may resist the repair process and thus may be responsible for causing the failure.
IV. Discussion
Sir Wilfred Fish,45in 1939, established that the root canal was a seat of infection. The pattern of osseous tissue breakdown in response to an irritant, coupled with microorganisms, such as that found in the periradicular bone in response to an infected root canal, was elegantly demonstrated by him. He drilled holes in the bones of guinea pigs and packed them with wool fibers saturated with microorganisms. Infected lesions were produced which exhibited four distinct, reactive zones: infection, contamination, irritation, and stimulation. The zone of infection was centrally located, exhibiting microorganisms and neutrophils. Immediately adjacent was the zone of contamination, characterized by a round-cell infiltrate. The zone of irritation contained histiocytes and osteoclasts. The outer zone of stimulation contained fibroblasts, new collagen, and initial osseous deposition.
The rationale for this approach is well established and is designed to minimize periradicular inflammation and promote healing.46Therefore, it can be presumed that if the root canal system is debrided thoroughly of all the necrotic material, release of toxic products to the apical area will cease and conditions favorable for repair of the periapical lesion will be created.5 In this study, only normal saline as irrigant and formocresol as antiseptic agent, were used, for obtaining an unbiased post-operative result as compared to other intracanal medicaments such as sodium hypochlorite (NaOCl) and chlorhexidine. Extrusion of NaOCl into periapical tissues can cause severe injury to the patient.47, 48Similarly,chlorhexidine cannot dissolve organic substances and necrotic tissues present in the root canal system and is unable to kill all bacteria and cannot remove the smear layer.49, 50Normal saline is an isotonic solution to the body fluids and is being universally used as an effective irrigating material in all the surgical procedures39 and has no side effects when used periapically.51-53Formocresol is one the oldest medicament used as antibacterial agent in the root canals and is still considered a gold standard by which all new modalities are compared.54 It was introduced to treat non-vital permanent teeth in the United States by Buckley in 1904.55 Studies have shown formocresol therapy to have a success rate between 70% and 90%.56 It is therefore both a potent bactericidal and devitalizing agent. It kills off and converts bacteria and pulp tissue into inert compounds.57Exogenous formaldehyde has a biologic half-life of 1-1.5 minutes and is quickly cleared from human plasma.58 When used judiciously, formocresol is a safe medicament.40
Certain manipulations may hasten regression of the pathosis and initiation of the reparative process. One such method was described by Bhaskar,19who suggested that whenever a periapical lesion is evident on a radiograph, instrumentation should be carried 1 mm beyond the apical foramen. This may cause transitory inflammation and, in addition, may cause subepithelial hemorrhage with ulceration of the epithelial lining, resulting in the resolution of the periapical lesion. The removal of the chronically inflamed periapical tissues improves the healing process of the lesion.10, 59

Bender (1972),60added that penetration of the apical area to the center of the radiolucency may help in resolution by establishing the drainage and relieving the pressure. Once the excess fluid is drained, fibroblasts begin to proliferate and deposit collagen; this compresses the capillary network, and epithelial cells are thus starved, undergo degeneration, and are engulfed by macrophages. Clinical success by these techniques has been claimed by Auslander, 1951 and Esposito, 1990.61-62
Bhaskar’s and Bender’s technique was based on the assumption that the periapical lesion could be a cyst. Even if the lesion is a granuloma or a chronic abscess, however, the same method can still prove effective, as it helps induce an acute transitory inflammatory reaction that may be followed by repair. Therefore, in the present study the said technique was employed during treatment of the cases.
The criteria for success used in this study were as follows: (1) tooth comfortable clinically, with no pain, tenderness, swelling, and mobility; and (2) elimination or decrease in size of periapical radiolucency or at least arrest of the lesion and no evidence of external root resorption on radiographs. Posttreatment, when the lesion is asymptomatic, it can also undergo fibrous healing or healing by formation of a scar. Radiographic examination reveals trabecular bone pattern radiating from the center but appears as an incompletely resolved radiolucency.63

Patients were recalled at intervals of 3 months, 6 months, 1 year, and 2 years. This is because, in order to assess the healing potential, at least a 6-month64 to 12-month65 period after root canal treatment should be considered. A 2-year follow-up period, according to Bender and colleagues,66is a reasonable time in which to arrive at a conclusion concerning success or failure. They observed that it may take up to 2 years for enough bone to be destroyed by an expanding granuloma or cyst to produce a change visible on radiographs.
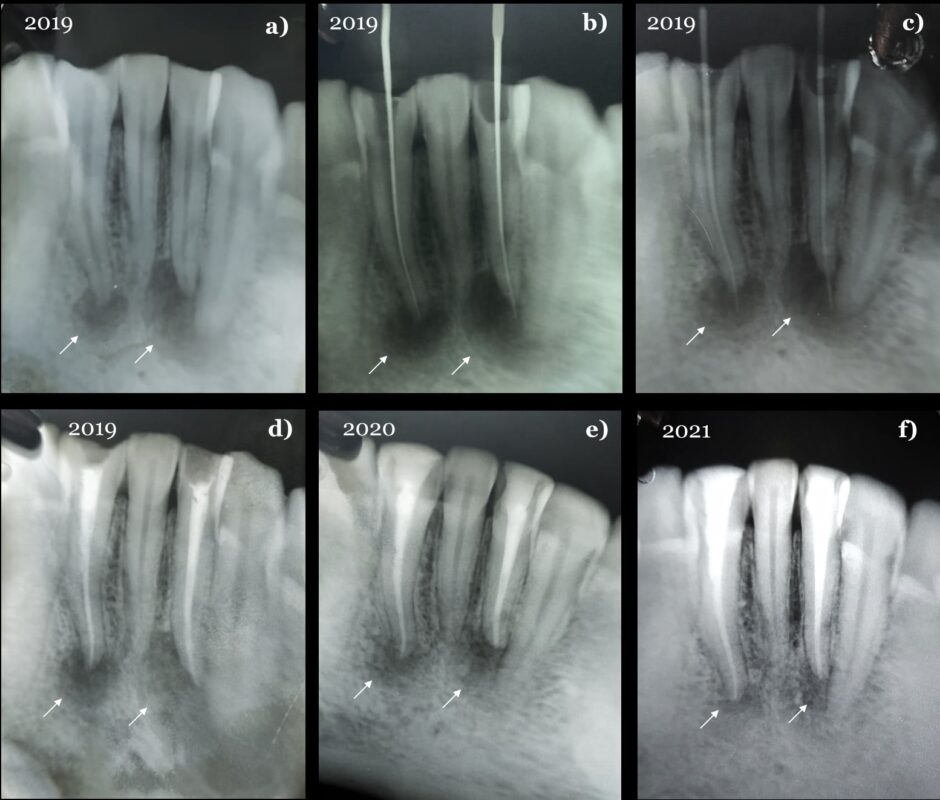
Of the 3 cases of treatment failure, 1 patient had to be treated by apical surgery immediately as they failed to respond to conservative management. Either the discharge from the canal persisted, pain or swelling developed after closed dressing, or the sinuses failed to heal. The other two cases of failure were interesting, as theyshowed an increasing area of periapical radiolucency on radiographs,1 year after completion of the treatment (Fig. 5). None of these patients had any acute symptoms.
In a retrospective study, Bence and coworkers,67reported a success rate of 82.2% with conservative endodontic management of 5000 teeth by three operators. In another study, Barbakow and associates,68reported a success rate of 89%, but their follow-up period was only one year. It is to be noted that 66.66% of the failures in the present study occurred 1 year after completion of treatment.
From the present study, the following observations are made:
- Conservative endodontic management is desirable in all cases, irrespective of age and sex, and is possible in a large percentage of cases (94% in this study). Therefore, an attempt must be made to treat patients conservatively as far as possible.
- The method of carrying the instrumentation to the center of the apical radiolucency was found effective in speeding the recovery and healing, but there is always the possibility that quiescent epithelial cells may be stimulated by instrumentation in the apical region, with resultant proliferation and cyst formation. Therefore, it is extremely essential to follow up all cases treated endodontically for a period of at least 2 years.
- NiTi hand-protaper instruments were found very convenient for mechanical preparation of the root canals. No breakage, perforation, and ledge formation, was encountered by the operator. In fact, access and visibility were much better and the risk of the instruments’ falling into the throat and being aspirated was completely eliminated with the placement of the rubber dam. As no pressure was required for mechanical cleansing with NiTi hand-protaper instruments, unlike standard hand instruments, fatigue was also reduced. NiTi protaper reamers and files exhibited good flexibility and took the shape of the canal without breaking.
- Ultimate success in the control of periapical infection, is the complete debridement of the root canal system, followed by three-dimensional obturation to seal both the apical foramen and coronal orifice.32
V. Conclusion
- A total of 50 teeth exhibiting signs and symptoms or radiographic evidence of periapical disease were treated endodontically, irrespective of the age and sex of the patients, and were followed up for a period of 2 years.
- Conservative management was successful in 94%, while 6% of the patients had to be subjected to surgery.
- Histopathologic examination of tissue specimens in unsuccessfully treated cases showed that all three consisted of chronic inflammatory tissue.
- Out of 3 failed cases, 2 (66.66%) occurred 1 year after completion of the treatment. Therefore, the need for long-term follow-up of treated endodontic cases is stressed.
- NiTi protaper instruments were found more convenient to use than standard hand instruments in clinical situations. Visibility and safety during handling were improved, and fatigue of the operator was reduced. These instruments exhibited good flexibility and minimized the chances of breakage within the canal.
However, further studies may be implemented for variable presentation of the periapical lesions, diagnosis and management. It is highly recommended that with technological advances, further minimally invasive approaches must be considered for resolving the issue of persistent periapical lesions, to reduce the burden for patients.69
Source of support: Nil
Conflict of interest: None declared
References
- Kakehashi S, Stanley HR, Fitzgerald RJ. The effects of surgical exposures of dental pulps in germ-free and conventional laboratory rats. Oral Surg Oral Med Oral Pathol. 1965;20:340–9.
- Möller AJ, Fabricius L, Dahlén G, Ohman AE, Heyden G. Influence on periapical tissues of indigenous oral bacteria and necrotic pulp tissue in monkeys. Scand J Dent Res. 1981;89(6):475–84.
- Ramachandran Nair PN. Light and electron microscopic studies of root canal flora and periapical lesions. J Endod. 1987;13(1):29–39.
- Lin LM, Huang GT, Rosenberg PA. Proliferation of epithelial cell rests, formation of apical cysts, and regression of apical cysts after periapical wound healing. J Endod. 2007 Aug;33(8):908-16. doi: 10.1016/j.joen.2007.02.006. Epub 2007 Apr 2. PMID: 17878074.
- Shah N. Nonsurgical management of periapical lesions: a prospective study. Oral Surg Oral Med Oral Pathol. 1988 Sep;66(3):365-71. doi: 10.1016/0030-4220(88)90247-2. PMID: 3174072.
- Hoen MM, LaBounty GL, Strittmatter EJ. Conservative treatment of persistent periradicular lesions using aspiration and irrigation. J Endod. 1990 Apr;16(4):182-6. doi: 10.1016/S0099-2399(06)81968-0. PMID: 2074410.
- Loushine RJ, Weller RN, Bellizzi R, Kulild JC. A 2-day decompression: a case report of a maxillary first molar. J Endod. 1991 Feb;17(2):85-7. doi: 10.1016/S0099-2399(06)81614-6. PMID: 1919408.
- Calişkan MK. Prognosis of large cyst-like periapical lesions following nonsurgical root canal treatment: a clinical review. Int Endod J. 2004 Jun;37(6):408-16. doi: 10.1111/j.1365-2591.2004.00809.x. PMID: 15186249.
- Er K, Kuştarci A, Ozan U, Taşdemir T. Nonsurgical endodontic treatment of dens invaginatus in a mandibular premolar with large periradicular lesion: a case report. J Endod. 2007 Mar;33(3):322-4. doi: 10.1016/j.joen.2006.09.001. Epub 2006 Nov 22. PMID: 17320725.
- Metzger Z, Huber R, Slavescu D, Dragomirescu D, Tobis I, Better H. Healing kinetics of periapical lesions enhanced by the apexum procedure: a clinical trial. J Endod. 2009 Feb;35(2):153-9. doi: 10.1016/j.joen.2008.11.019. Epub 2008 Dec 12. PMID: 19166763.
- Friedman S, Lustmann J, Shaharabany V. Treatment results of apical surgery in premolar and molar teeth. J Endod. 1991;17(1):30–3.
- Frank AL, Glick DH, Patterson SS, Weine FS. Long-term evaluation of surgically placed amalgam fillings. J Endod. 1992;18(8):391–8.
- Kvist T, Reit C. Results of endodontic retreatment:a randomized clinical study comparing surgical and nonsurgical procedures. J Endod. 1999;25(12):814–7.
- Rud J, Andreasen JO, Jensen JE. A follow-up study of 1,000 cases treated by endodontic surgery. Int J Oral Surg. 1972;1(4):215–28.
- Kettering JD, Torabinejad M, Jones SL. Specificity of antibodies present in human periapical lesions. J Endod. 1991;17(5):213–6.
- Kim S. Principles of endodontic microsurgery. Dent Clin North Am. 1997;41(3):481–97.
- Sood N, Maheshwari N, Gothi R, Sood N. Treatment of large periapical cyst like lesion: A noninvasive approach: A report of two cases. Int J Clin Pediatr Dent 2015;8:133-7.
- Seltzer S, Bender B, Nazimov H, et al. Pulpitis-induced interradicular periodontal changes in experimental animals. J Periodontol. Mar-Apr 1967;38(2):124-9. doi: 10.1902/jop.1967.38.2.124.
- Bhaskar SN. Nonsurgical resolution of radicular cysts. ORAL SURG ORAL MED ORAL PATHOL 1972;34:458-68.
- Bonaccorso A, Tripi TR. Endo-perio lesion: Diagnosis, prognosis and decision-making. ENDO (Lond Engl). 2014;8(2):105–127.
- Lalonde ER, Luebke RG. The frequency and distribution of periapical cysts and granulomas. Oral Surgery, Oral Medicine and Oral Pathology. 1968; 25, 861-8.
- Sargenti A. Case reports: diagnosing, treating radicular cysts. Dental Survey. 1973; 49, 2 2-4.
- Wood NK. Periapical lesions. Dental Clinics of North America. 1984; 28, 725-66.
- Mumford JM, Jedynakiewicz NM. Principles of Endodontics. London, DK: Quintessence Publishing Co. Ltd. 1988; 161.
- Stockdale CR, Chandler NP. The nature of the periapical lesion—a review of 1108 cases. Journal of Dentistry. 1988; 16, 123-9.
- Mangani F. Il trattamentoortogrado dele grandilesioni di origineendodontica: contributoclinicostatistico. Giarinak Italiano di Endodonzia. 1990; 4, 8-13.
- Huang HY, Chen YK, Ko EC, Chuang FH, Chen PH, Chen CY, et al. Retrospective analysis of nonendodontic periapical lesions misdiagnosed as endodontic apical periodontitis lesions in a population of Taiwanese patients. Clin Oral Investig2017;21:2077-82.
- Oztan MD. Endodontic treatment of teeth associated with a large periapical lesion. Int Endod J 2002;35:73-8.
- Sena Guimarães AL, Marques-Silva L, Cavaliéri Gomes C, Castro WH, Mesquita RA, Gomez RS. Peripheral brown tumour of hyperparathyroidism in the oral cavity. Oral Oncol Extra 2006;42:91-3.
- Saunders EM. Hand instrumentation in root canal preparation. Endodontic Topics. 2005 March;10(1):163 – 167.
- Hülsmann M, Stryga F. Comparison of root canal preparation using different automated devices and hand instrumentation. J Endod. 1993 Mar;19(3):141-5. doi: 10.1016/S0099-2399(06)80509-1. PMID: 8509753.
- Maalouf EM, Gutmann JL. Biological perspectives on the non-surgical endodontic management of periradicular pathosis. Int Endod J. 1994 May;27(3):154-62. doi: 10.1111/j.1365-2591.1994.tb00246.x. PMID: 7995649.
- Farman AG, Kolsom SA. Intraoral Radiographic Techniques. Available from: http://www.dentalcare.com/en-US/dental-education/continuing-education/ce119/ce119.aspx? review=true.
- Gupta, A., Devi, P., Srivastava, R., & Jyoti, B. (2014). Intra oral periapical radiography – basics yet intrigue: A review. Bangladesh Journal of Dental Research & Education, 4(2), 83-87. https://doi.org/10.3329/bjdre.v4i2.20255.
- Natkin E. Oswald RJ, Carnes LI. The relationship of lesion size to diagnosis, incidence, and treatment of periapical cysts and granulomas. Oral Surgery. Oral Medicine and Oral Pathology. 1984;57, 82-94.
- Das S. A manual on clinical surgery- 9th edition. 2011 August.
- Grossman LI. Textbook of ‘Endodontic Practice’. 13th Ed.
- White SC, Pharoah MJ. Textbook of ‘Oral Radiology- Principles and Interpretation’. 6th Ed.
- Shahid Shuja Qazi ,Manzoor Ahmed Manzoor ,Rizwan Oureshi ,Hannan Humayun Khan , Comparison of postoperative pain – normal saline vs sodium hypochlorite as irrigants, Pak. Oral Dent. J. 2005; 25 (2): 177-182.
- Chandrashekhar S, Shashidhar J. Formocresol, still a controversial material for pulpotomy: A critical literature review. J Res Dent. 2014;2:114-24.
- Roane JB, Sabala CL, Duncanson MG Jr. The ‘balanced force’ concept for instrumentation of curved canals. J Endod. 1985; 11: 203–211.
- Roane JB, Sabala CL. Clockwise or counterclockwise? J Endod. 1984; 10: 349–353.
- Hülsmann M, Peters OA, Dummer PMH. Mechanical preparation of root canals: Shaping goals, techniques and means. Endodontic Topics. 2005 March;10(1):30 – 76.
- Prader F. Diagnose und Therapie des InfiziertenWurzelkanales. Basel: Benno Schwabe, 1949.
- Fish EW. Bone infection. J Am Dent Assoc 1939; 26:691-712.
- Gutmann JL, Dumsha TC. Cleaning and shaping the root canal system. In: Cohen S, Burns R. eds. Pathways of the Pulp. 4th edn. St Louis, MO, DSA: CV Mosby Co. 1987; 156-82.
- Hülsmann M, Hahn W. Complications during root canal irrigation—literature review and case reports. Int Endod J 2000;33:186-93.
- Reeh ES, Messer HH. Long-term paresthesia following inadvertent forcing of sodium hypochlorite through perforation in maxillary incisor. Endod Dent Traumatol1989;5:200-3.
- Estrela C et al. Efficacy of sodium hypochlorite and chlorhexidine against Enterococcus faecalis—a systematic review. J Appl Oral Sci 2008;16:364-8.
- Shabahang S, Aslanyan J, Torabinejad M. The substitution of chlorhexidine for doxycycline in MTAD: the antibacterial efficacy against a strain of Enterococcus faecalis. J Endod2008;34:288-90.
- Weber C, McClanahan S, Miller G, Diener-West M, Johnson J. The effect of passive ultrasonic activation of 2% chlorhexidine or 5.25% sodium hypochlorite irrigant on residual antimicrobial activity in root canals. J Endodon 2003;29(9):562-564.
- Short R, Dom SO, Kuttler S. The crystallization of sodium hypochlorite on gutta-percha cones after the rapid-sterilization technique: an SEM study. J Endodon 2003;29(10):670-673.
- Sabins R, Johnson J, Hellstein J. A comparison of the cleaning efficacy of short-term sonic and ultrasonic passive irrigation after hand instrumentation in molar root canals. J Endodon 2003;29(10):674-678.
- Fei AL, Udin RD, Johnson R. A clinical study of ferric sulfate as a pulpotomy agent in primary teeth. Pediatr Dent.1991; 13:327-32.
- Ranly DM. Pulpotomy therapy in primary teeth: New modalities for old rationales. Pediatr Dent.1994; 16:403-9.
- Wright FA, Widmer RP. Pulpal therapy in primary molar teeth: A retrospective study. J Pedod.1979; 3:195-206.
- Restorative techniques in paediatric dentistry. In: Duggal MS, editor. 2nd ed. 2002; 50-63.
- Bhatt HS, Lober SB, Combes B. Effect of glutathione depletion on aminopyrine and formaldehyde metabolism. BiochemPharmacol.1988; 37:1581-9.
- Metzger Z, Huber R, Tobis I, Better H. Enhancement of healing kinetics of periapical lesions in dogs by the Apexum procedure. J Endod. 2009;35(1):40–5.
- Bender IB. Commentary on General Bhaskar’s hypothesis, ORAL SURG ORAL MED ORAL PATHOL 1972:34:469-76.
- Auslander WP. Root canal therapy technic for general practitioners. New York Journal of Dentistry. 1951;21. 451-4.
- Esposito JV. Apical violation in periapical ‘area’ cases—blasphemy or therapy? Dental Clinics of North America. 1990;34, 171-8.
- Chong BS. Managing Endodontic Failure. Chicago: Quintessence Pub.; 2004.
- Torres-Lagares D, Segura-Egea JJ, Rodríguez-Caballero A, Llamas-Carreras JM, Gutiérrez-Pérez JL. Treatment of a large maxillary cyst with marsupialization, decompression, surgical endodontic therapy and enucleation. J Can Dent Assoc. 2011;77:b87.
- Orstavik D. Time-course and risk analyses of the development and healing of chronic apical periodontitis in man. Int Endod J. 1996;29(3):150–5.
- Bender IB, Seltzer S, Soltanoff W. Endodontic success-a reappraisal of criteria. ORAL SURG ORAL MED ORAL PATHOL 1966;22:780-802.
- Bence R, Meyers RD, Knoff RV. Evaluation of 5000 endodontic treatments: incidence of the opened tooth. ORAL SURG ORAL MED ORAL PATHOL 1980;49:82-4.
- Barbakow FH, Cleaton-Jones PE, Friedman D. Endodontic treatment of teeth with periapical radiolucent areas in a general dental practice. ORAL SURG ORAL MED ORAL PATHOL 1981;51:552-9.
- Karamifar K, Tondari A, Saghiri MA. Endodontic Periapical Lesion: An Overview on the Etiology, Diagnosis and Current Treatment Modalities. Eur Endod J. 2020 Jul 14;5(2):54-67. doi: 10.14744/eej.2020.42714. PMID: 32766513; PMCID: PMC7398993.

 Click here for Dental Services
Click here for Dental Services
Well explained…
Must say Informative and accurate too.