POST-COVID SYNDROME AND LONG COVID
Experience of signs and symptoms, and development of long term multi-organ complications after Covid-19 affliction is termed as Long Covid Syndrome.
Blog By: Dr. Shivangi Singla
![]() TRUE VALUE DENTAL INSTITUTE
TRUE VALUE DENTAL INSTITUTE
Introduction
he SARS-CoV-2 virus infects humans via droplets, and to some extent, aerosols.1 In symptomatic adults, the disease typically presents after 2–14 days of incubation as a respiratory illness with fever, cough, headache, myalgia and in some cases intestinal symptoms.2 However, it is now also clear that some individuals with milder initial symptoms of COVID-19 can suffer from variable and debilitating symptoms for many months after the initial infection.3, 4 The substantivity of the coronavirus in the body depends upon person to person, exposure to the virus and severity of infection. This may mean some people get a second positive test result even after they recover, although this does not necessarily indicate the virus is still transmissible.
What is Post Covid Syndrome or Long Covid?
Most people infected with COVID-19 infection get better within 10 days of illness. After a long period of intensive care and mechanical ventilation, general anesthesia and severe illness, it is not surprising that long rehabilitation periods are needed.5 An exact definition is lacking, but typically symptoms with a duration >2 months are considered Long Covid.6
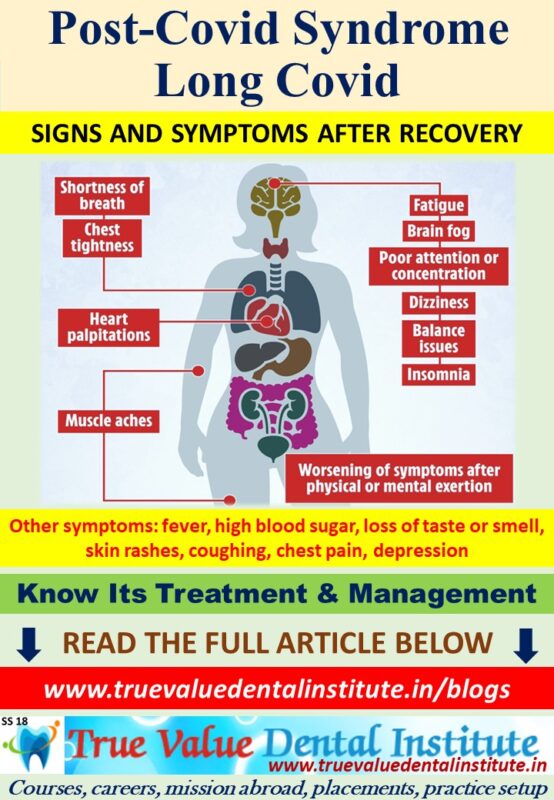
People when continue to experience mild symptoms post recovery are popularly considered to have Post Covid Syndrome or Long Covid.
These people may experience post-covid conditions and also develop long-term complications that affect the organs. Post-covid complications are a broad range of new, ongoing or returning health conditions, people can experience more than 28 days / 4 weeks after first being infected with the coronavirus. Even asymptomatic people who did not have symptoms when they were infected can have post COVID complications. The condition involves a range of symptoms such as persistent fatigue, myalgia, autonomic dysregulation manifested as postural orthostatic tachycardia syndrome, abnormal thermoregulation, intestinal disturbances and skin manifestations.7
Resemblance with other diseases
This post-COVID syndrome bears resemblance to postinfectious syndromes that followed outbreaks of chikungunya8 and Ebola9, for example, and selected symptoms overlap with myalgic encephalomyelitis, a disease that is also often triggered by infection and immune activation10 and manifests as a dysregulated autonomic nervous system and perturbed immune parameters11.
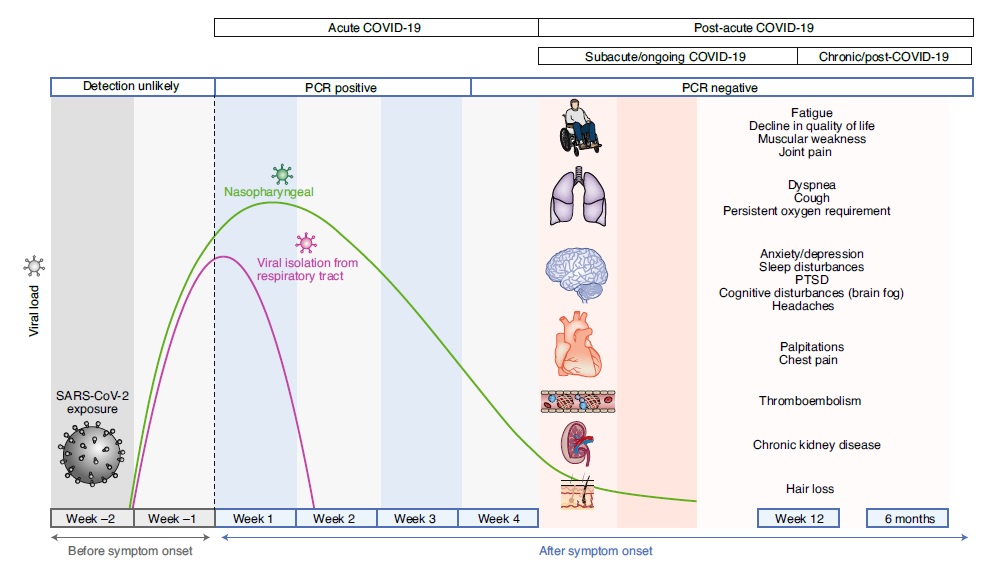
Timeline of Post-Acute Covid-1912
Acute COVID-19 usually lasts until 4 weeks from the onset of symptoms, beyond which replication-competent SARS-CoV-2 has not been isolated. Post-acute COVID-19 (Long Covid) is defined as persistent symptoms and/or delayed or long-term complications beyond 4 weeks from the onset of symptoms. The common symptoms observed in post-acute COVID-19 are summarized.
Pathophysiology of Long Covid
The predominant pathophysiologic mechanisms of acute COVID-19 include the following: direct viral toxicity; endothelial damage and microvascular injury; immune system dysregulation and stimulation of a hyperinflammatory state; hypercoagulability with resultant in situ thrombosis and macrothrombosis; and maladaptation of the angiotensin-converting enzyme 2 (ACE2) pathway.13
Potential mechanisms contributing to the pathophysiology of post-acute COVID-19 include:14-18
(1) virus-specific pathophysiologic changes;
(2) immunologic aberrations and inflammatory damage in response to the acute infection; and
(3) expected sequelae of post-critical illness à includes new or worsening abnormalities in physical, cognitive and psychiatric domains after critical illness.
The pathophysiology of post-intensive care syndrome is multifactorial and has been proposed to involve microvascular ischemia and injury, immobility and metabolic alterations during critical illness.16 Additionally, similar to previous studies of SARS survivors, 25–30% of whom experienced secondary infections,19-20 survivors of acute COVID-19 may be at increased risk of infections with bacterial, fungal (pulmonary aspergillosis) or other pathogens.21-23 However, these secondary infections do not explain the persistent and prolonged sequelae of post-acute COVID-19.
Symptoms of Long covid24
- Cardiovascular à chest-burn, tachycardia, palpitations, fainting etc.
- Dermatologic à skin rashes, itching, petechiae, peeling skin etc.
- Gastrointestinal à GERD, diarrhea, loss of appetite, vomiting etc.
- Head, ear, eye, nose, throat (HEENT) à sore throat, blurred vision, tinnitus, running nose etc.
- Immunologic autoimmune à allergy, shingles, lymphadenopathy etc.
- Musculoskeletal à tightness of chest, muscles of chest, muscle spasms, joint pain etc.
- Neuropsychiatric à mood changes, memory loss, brain fog, tremors, insomnia etc.
- Pulmonary, respiratory à breathing difficulty, sneezing, dry cough, hemoptysis etc.
- Reproductive, genitourinary, endocrine à extreme thirst, menstrual issues, sexual dysfunction, bladder control issues etc.
- Systemic à febrile, fatigue, malaise, weakness etc.
- MISC-C12 à multisystem inflammatory syndrome in people <21 years old.
Triggers for relapses/worsening of symptoms24
- Stress
- Alcohol
- Caffeine
- Heat
- Exercise
- Physical activity
- Mental activity
- Menstruation
- Any other infection or aggravation
Conclusion
This suggests that Long COVID is composed of heterogeneous sequelae that often affect multiple organ systems, with impact on functioning and ability to work. Patients with COVID-19 develop an array of symptoms that evolve over time. Recognizing the persistence of symptoms could legitimize patients’ concerns in an unknown and new disease. Adequate communication can provide reassurance, reduce anxiety, and potentially optimize recovery.
References
- Van Doremalen, N. et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N. Engl. J. Med. 2020; 382: 1564–1567
- Huang, C. et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020; 395: 497–506
- Dennis, A. et al. Multi-organ impairment in low-risk individuals with long COVID. Preprint at medRxiv. 2020. https://doi.org/10.1101/2020.10.14.20212555
- Ludvigsson, J. F. Case report and systematic review suggest that children may experience similar long‐term effects to adults after clinical COVID‐19. Acta Paediatr. 2020. https://doi.org/10.1111/apa.15673
- Carfì, A. et al. Persistent symptoms in patients after acute COVID-19. JAMA. 2020; 324: 603–605
- Brodin P. Immune determinants of COVID-19 disease presentation and severity. Nature Medicine. January 2021; 27:28-33
- Davido, B., Seang, S., Tubiana, R. & de Truchis, P. Post-COVID-19 chronic symptoms: a post-infectious entity? Clin. Microbiol. Infec. 2020; 26: 1448–1449
- Guillot, X., Ribera, A. & Gasque, P. Chikungunya-induced arthritis in Reunion Island: a long-term observational follow-up study showing frequently persistent joint symptoms, some cases of persistent chikungunya immunoglobulin M positivity, and no anticyclic citrullinated peptide seroconversion after 13 years. J. Infect. Dis.2020; 222: 1740–1744
- Clark, D. V. et al. Long-term sequelae after Ebola virus disease in Bundibugyo, Uganda: a retrospective cohort study. Lancet Infect. Dis. 2015; 15: 905–912
- Hickie, I. et al. Post-infective and chronic fatigue syndromes precipitated by viral and non-viral pathogens: prospective cohort study. BMJ. 2006; 333, 575
- Rodriguez, L. S. T. et al. Achieving symptom relief in patients with Myalgic encephalomyelitis by targeting the neuro-immune interface and inducing disease tolerance. Preprint at bioRxiv. 2020. https://doi.org/10.1101/2020.02.20.958249
- Nalbandian, A., Sehgal, K., Gupta, A. et al. Post-acute COVID-19 syndrome. Nat Med 27, 601–615 (2021). https://doi.org/10.1038/s41591-021-01283-z
- Gupta, A. et al. Extrapulmonary manifestations of COVID-19. Nat. Med. 26, 1017–1032 (2020).
- Needham, D. M. et al. Physical and cognitive performance of patients with acute lung injury 1 year after initial trophic versus full enteral feeding. EDEN trial follow-up. Am. J. Respir. Crit. Care Med. 188, 567–576 (2013).
- Pandharipande, P. P. et al. Long-term cognitive impairment after critical illness. N. Engl. J. Med. 369, 1306–1316 (2013).
- Inoue, S. et al. Post-intensive care syndrome: its pathophysiology, prevention, and future directions. Acute Med. Surg. 6, 233–246 (2019).
- Kress, J. P. & Hall, J. B. ICU-acquired weakness and recovery from critical illness. N. Engl. J. Med. 370, 1626–1635 (2014).
- Hosey,M. M. & Needham, D. M. Survivorship after COVID-19 ICU stay. Nat. Rev. Dis. Prim. 6, 60 (2020).
- Zahariadis, G. et al. Risk of ruling out severe acute respiratory syndrome by ruling in another diagnosis: variable incidence of atypical bacteria coinfection based on diagnostic assays. Can. Respir. J. 13, 17–22 (2006).
- Zheng, Z., Chen, R. & Li, Y. The clinical characteristics of secondary infections of lower respiratory tract in severe acute respiratory syndrome. Chin. J. Respir. Crit. Care Med. 2, 270–274 (2003).
- Huang, C. et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 395, 497–506 (2020).
- Lescure, F. X. et al. Clinical and virological data of the first cases of COVID-19 in Europe: a case series. Lancet Infect. Dis. 20, 697–706 (2020).
- Zhou, F. et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 395, 1054–1062 (2020).
- H.E. Davis et al., Characterizing long COVID in an international cohort: 7 months of symptoms and their impact, EClinicalMedicine (2021), https://doi.org/10.1016/j.eclinm.2021.101019

 Click here for Dental Services
Click here for Dental Services